January 23, 2026
•
5 min read
How to Appeal Insurance Claim Denial A Guide for Expats
Learn how to appeal insurance claim denial with this guide for expats. Discover actionable steps and real-world tips to turn a denial into an approval.
Getting that dreaded claim denial notice when you're living abroad is beyond frustrating, but it's rarely the final word. A lot of those initial denials can be turned around with a strategic appeal, transforming a major headache into something you can absolutely handle.
The trick is to see this not as a fight, but as a structured conversation with your insurance provider. You just need a plan.
Your Roadmap to Overturning a Claim Denial
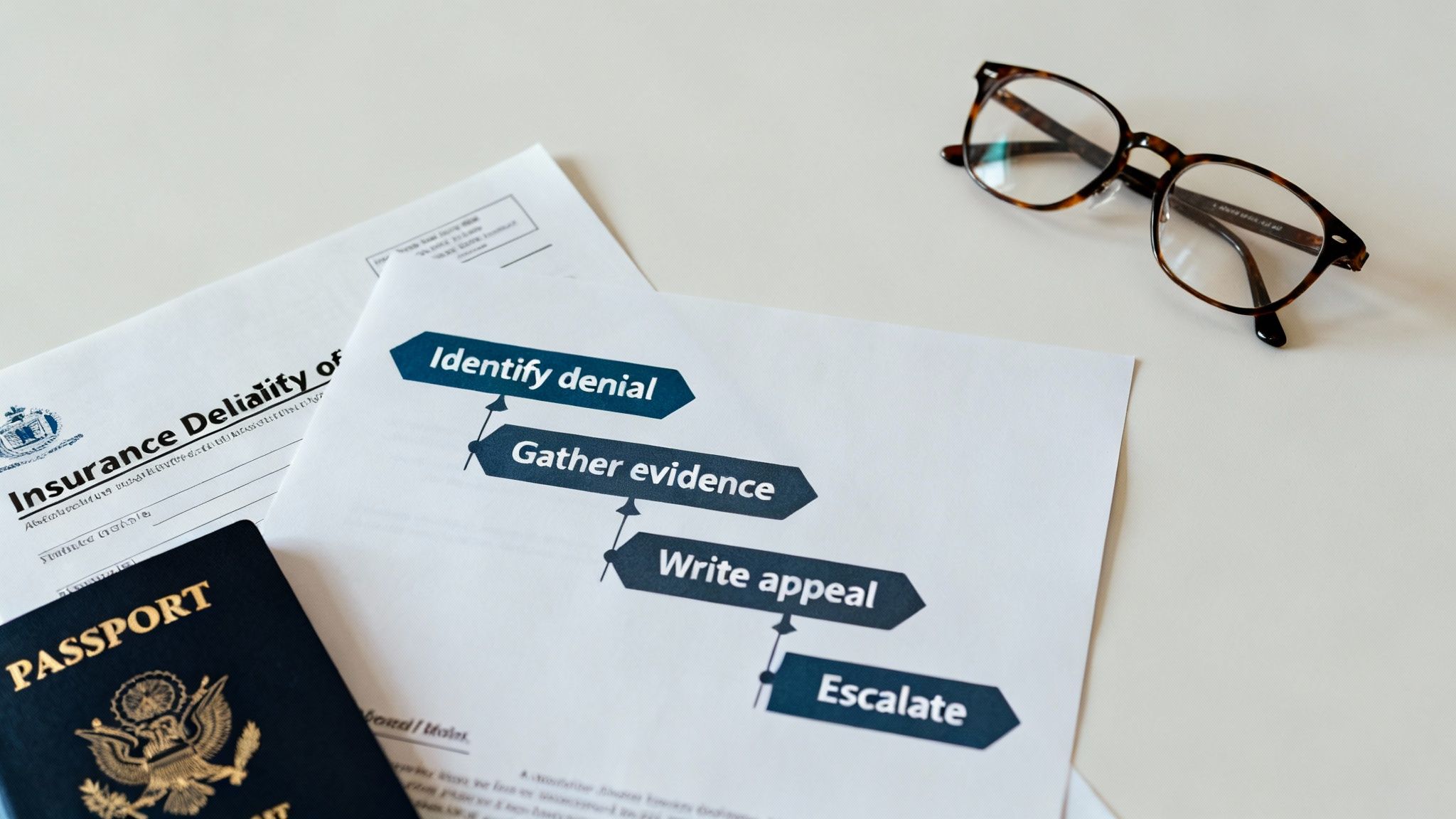
This guide will break down the whole process, giving you the confidence and the tools to challenge the insurer's decision. We’re going to walk through:
- Pinpointing the exact reason for the denial.
- Gathering the right evidence to build a rock-solid case.
- Crafting an appeal letter that is professional and persuasive.
The Reality of Claim Denials for Expats
Imagine you're an expat in Thailand. You have a motorcycle accident, end up with a hefty hospital bill, and then your insurer denies the claim for 'lack of prior authorization.' It’s a gut-punch, but you're not alone.
Statistics show that nearly 15% of all claims sent to private payers get denied right off the bat. For certain plans, that number can climb even higher, proving denials are a common hurdle even for those with what they believe is solid https://www.expatinsurance.com/articles/what-is-international-health-insurance.
For expats, dealing with this from another country adds a whole new layer of complexity. You're juggling time zones, potential language barriers, and unfamiliar medical systems. These things can easily lead to simple clerical errors, which—believe it or not—are behind a huge number of successful appeals.
Here's the good news: persistence really does pay off.
Shockingly, less than 1% of denied claims are ever actually appealed. But for those who do fight back, the success rate is impressive. Hospitals report that 50% of initial claim denials are overturned after an appeal. For a detailed breakdown, this guide on how to appeal an insurance claim denial offers some fantastic steps.
The financial stakes are high, but so are your odds of winning when you're prepared. Don't let yourself be among the 99% who just give up.
Decoding Your Denial Letter to Build a Strong Case
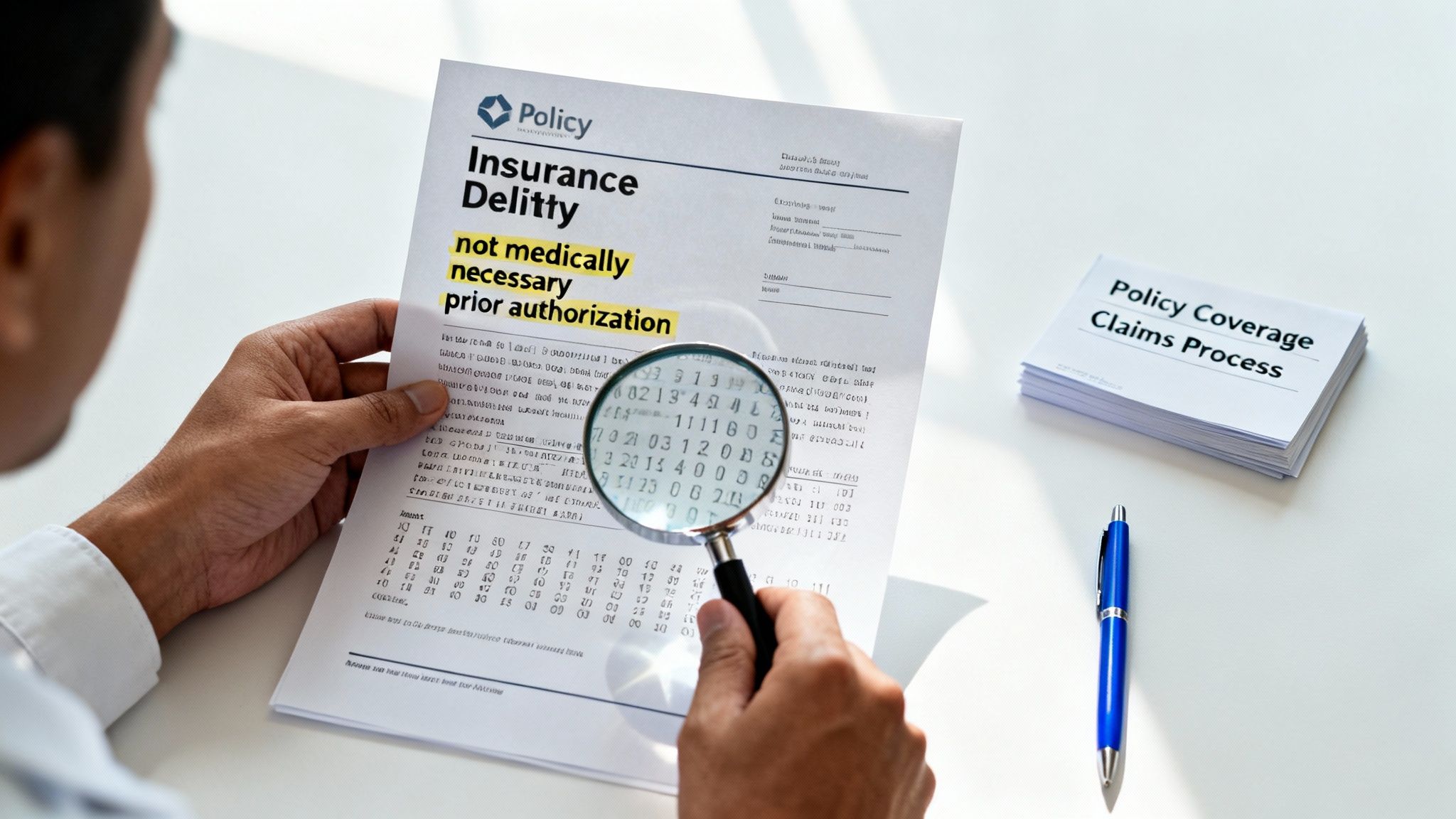
When a denial letter lands in your inbox, the natural first reaction is a mix of frustration and panic. My advice? Take a deep breath. That letter isn't the final word; it's your strategic playbook. It holds the exact reason your insurer said "no," and understanding that is the foundation of any successful appeal.
Your denial letter is a formal document that's required to explain the decision. Your job is to look for the specific terminology and reason codes they use. This isn't just industry jargon—these are direct clues that tell you precisely what kind of evidence you’ll need to gather to fight back effectively.
Finding the Core Reason for Denial
Insurers tend to use standardized language to justify their decisions. As an expat, you’re likely to run into a few common reasons, and they can range from a simple typo to a more complex disagreement over your treatment.
Your mission is to figure out which category your denial falls into. Was it a simple clerical error, like a misspelled name or an incorrect policy number? Or is it a more substantial issue, like a claim that your treatment was "not medically necessary"?
Pro Tip: Don't just skim the letter. Read every single line, paying close attention to any mention of your policy's specific clauses or exclusions. This is where the insurer lays out their case, and it's exactly where you'll find the weak points to target in your appeal.
A denial for a coding error, for instance, requires a completely different strategy than one for using an out-of-network provider. The first might just need a quick phone call to your doctor's billing department. The second, however, requires you to prove why you had to go outside the network—perhaps it was an emergency or there were no local specialists available.
Common Denial Reasons and Your First Action Step
Getting a handle on these common reasons is the key to moving forward. An administrative slip-up is often a quick fix, but a denial based on medical necessity will demand a much stronger argument, usually with direct support from your doctor.
Here's a quick breakdown of what you might see and what to do first.
| Denial Reason | What It Means | Your First Action Step |
|---|---|---|
| Administrative Error | A simple mistake was made on the claim form, such as a wrong birthdate, policy number, or service date. | Contact your medical provider's billing office to confirm the information submitted and ask them to refile a corrected claim immediately. |
| Out-of-Network Provider | You received care from a doctor or facility that is not part of your insurer’s approved network. | Review your policy for out-of-network benefits. If care was for an emergency, gather documents to prove it was your only option. |
| Not Medically Necessary | The insurer has determined the service you received was not essential for your diagnosis or treatment according to their guidelines. | Request a detailed "Letter of Medical Necessity" from your doctor that explains why the treatment was crucial for your health. |
| Lack of Prior Authorization | Your treatment required pre-approval from the insurer before it was performed, and this step was missed. | Speak with your doctor’s office to understand why pre-authorization wasn't obtained and if a retroactive authorization is possible. |
Knowing these distinctions shapes your entire strategy. Once you can pinpoint the why behind the denial, you move past the initial frustration and can start building a logical, focused case.
Sometimes, a denial is also related to policy specifics like deductibles or waiting periods. If you're wrestling with shared cost terms, our guide can help you understand what coinsurance in health insurance means and how it affects your claims. By dissecting that denial letter, you’re already one step closer to getting it overturned.
Gathering Your Evidence for a Winning Appeal
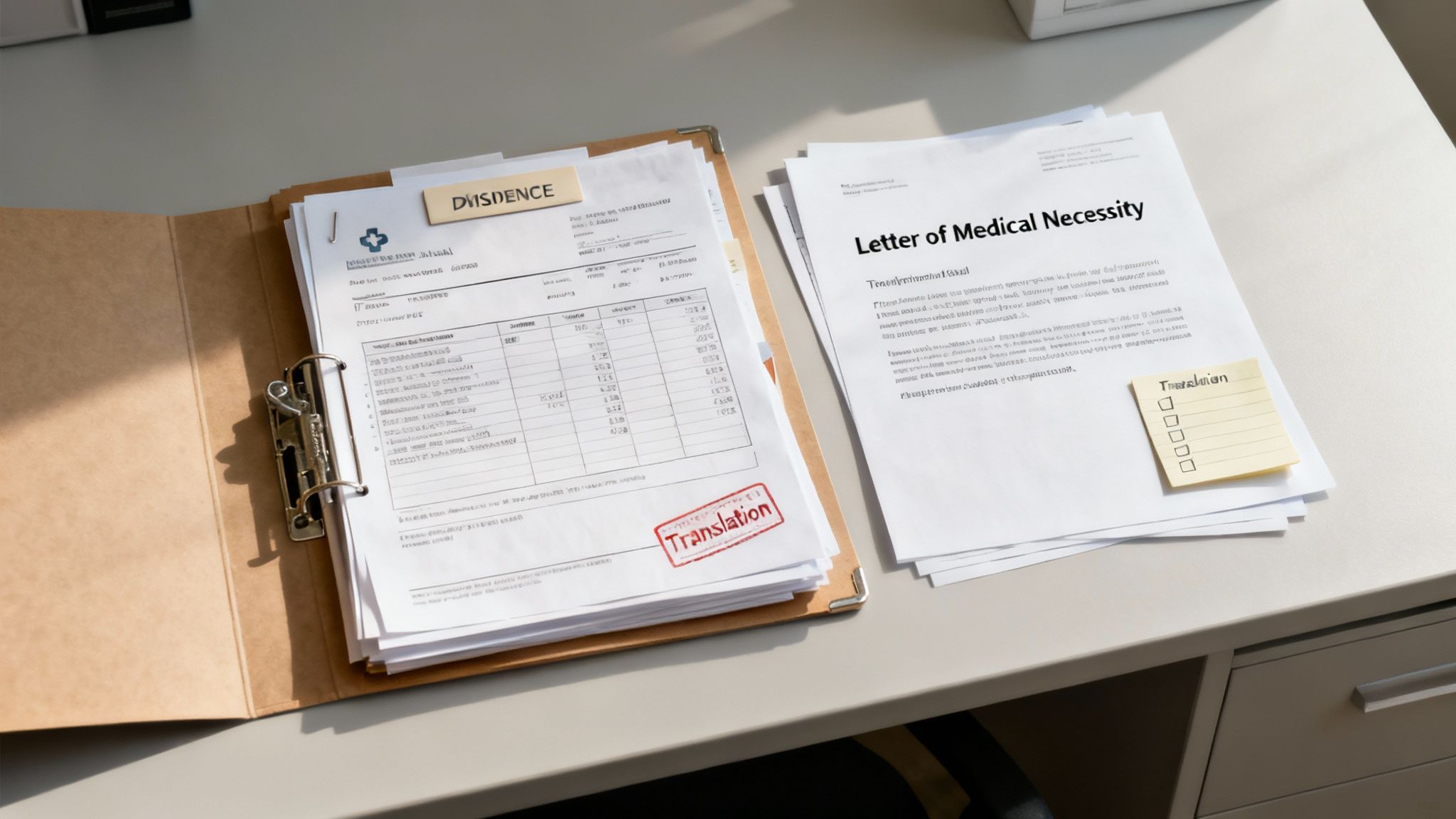
Once you understand why your claim was denied, it's time to build an undeniable case. Let's be clear: a successful appeal isn't about emotion. It's about presenting cold, hard facts that directly counter the insurer's reason for the denial, leaving them very little room to argue.
Think of yourself as a detective. Every document you find is a piece of the puzzle, making it that much harder for the claims reviewer to say "no" a second time.
Your Essential Document Checklist
First things first, get organized. Create a central folder—either a physical one or a digital one on your computer—for absolutely everything related to this claim. A messy, incomplete submission is just asking for another denial.
Your evidence file needs to include:
- The Original Denial Letter: This is your roadmap. It tells you exactly which argument you need to dismantle.
- Your Original Claim Submission: Keep a copy of the initial claim and every single document you sent along with it.
- All Communication with the Insurer: This means records of phone calls (date, time, who you spoke to, a quick summary) and copies of every email or letter.
- Your Insurance Policy Document: Find and highlight the specific sections that cover the denied service. This proves you've done your homework.
This foundational paperwork sets the stage for the most important part of your evidence gathering: your medical documentation.
The Power of Medical Records
Your medical file is the heart and soul of your appeal, especially for those frustrating "not medically necessary" denials. Vague summaries just won't cut it here. You need detailed, official records that paint the complete picture of your health situation.
Get in touch with your doctor or hospital and request a complete copy of your medical records. For denials related to your health, a healthcare medical record analyzer can be a surprisingly useful AI tool for quickly sifting through your history to find the crucial bits of information that support your case.
Your medical evidence package absolutely must include:
- Physician’s Notes: These are the clinical notes that detail your symptoms, diagnosis, and your doctor's reasoning.
- Test and Lab Results: Any diagnostic imaging, blood work, or other tests that back up your condition.
- Itemized Bills: Don't just send the summary. You need the detailed breakdown of every single service and supply you were billed for.
One of the single most powerful documents you can get is a Letter of Medical Necessity. This is a formal letter written by your doctor explaining, in professional terms, why the treatment or medication wasn't just helpful—it was essential for your health.
Navigating Expat-Specific Hurdles
As an expat, this part can get tricky. What if your doctor in Portugal only keeps records in Portuguese? An insurer is well within their rights to reject documents they can't read.
It's on you to provide certified translations of key documents, like that all-important Letter of Medical Necessity. Please don't rely on free online tools for this; it's worth investing in a professional translation service to ensure everything is accurate and credible. If you're hitting a language barrier just trying to request the records, a bilingual friend, a local facilitator, or your Expat Insurance broker can be a true lifesaver.
This effort pays off. Astonishingly, some studies show that nearly 99% of denials go unchallenged. But here's the kicker: hospitals that do appeal manage to overturn 50% of initial denials. This proves that a well-supported case has a real fighting chance.
Building your evidence file is methodical, painstaking work, but it's the most critical step you'll take. A thorough, organized file makes your argument professional, credible, and very difficult to ignore. Also, a solid grasp of your policy's cost-sharing rules can prevent future issues; for a refresher, check out our guide on understanding health insurance deductibles.
How to Write a Compelling Insurance Appeal Letter
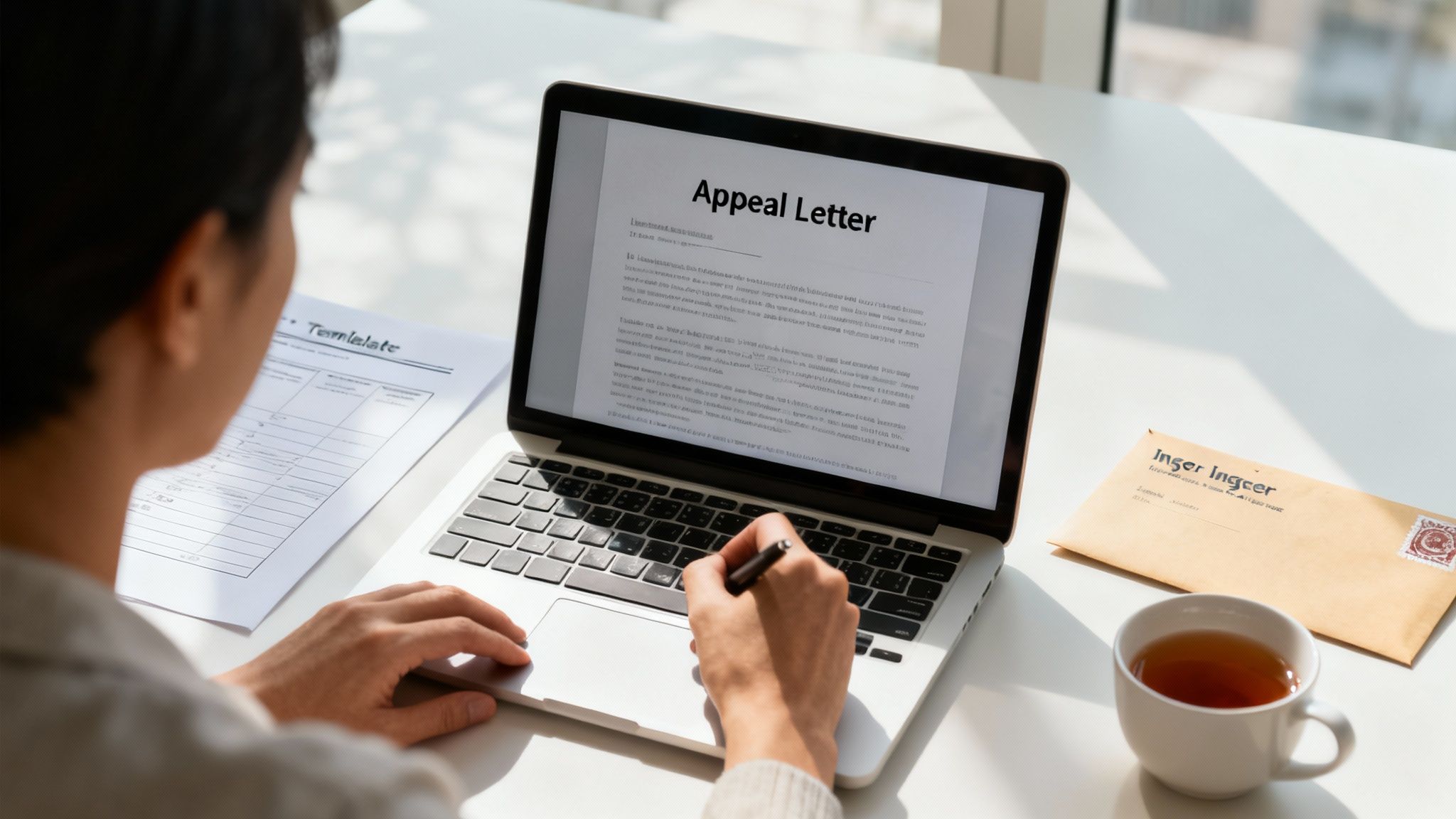
After you've meticulously gathered all your evidence, the next move is to channel it into a clear, professional, and persuasive appeal letter. This document is the heart of your argument—your formal request for the insurer to take a second look.
This isn't the place to vent your anger or frustration. Your letter needs to be a logical, fact-based story that makes it dead simple for the reviewer to understand your point of view and, hopefully, overturn the denial.
Just picture the person on the other end. They're likely sifting through dozens of cases a day, looking for a straightforward, evidence-backed reason to say "yes." Your job is to give them exactly that.
Structuring Your Appeal for Maximum Impact
A well-structured letter is your roadmap, guiding the reviewer through your case step-by-step. I've seen too many people rush this part, ending up with a jumbled mess that guarantees another rejection. A confusing letter forces the reviewer to connect the dots, and frankly, they just don't have the time.
Start with the basics. Put your full name, policy number, and claim number right at the top. It seems obvious, but you'd be surprised how often it's missed. From there, your letter should follow a clear, four-part flow.
- Quick Intro: Get straight to the point.
- Factual Summary: Give a brief timeline of what happened.
- Point-by-Point Rebuttal: Tackle the exact reason for the denial.
- Clear Conclusion: Tell them exactly what you want.
This framework elevates your appeal from a simple complaint to a professional dispute that has to be taken seriously.
An effective appeal letter is respectful but firm. Think business letter, not personal grievance. Remember, the claims reviewer didn't personally deny your claim; they’re just the person tasked with re-evaluating it based on the new facts you provide.
Crafting Each Section of Your Letter
Alright, let's get into the nuts and bolts of what makes each section of the letter work. The details are everything here—vague statements are the fastest way to get your appeal tossed aside.
The Introduction and Factual Summary
Your opening needs to be direct. Something like, "I am writing to formally appeal the denial of claim number [Your Claim Number] for services received on [Date of Service]." No fluff, just facts. It immediately sets a professional tone.
Next, give a short, chronological summary of the events. This isn't where you launch into detailed medical arguments. It’s a simple recap to set the stage. For instance, explain when you first saw a doctor, the diagnosis, and the recommended treatment.
The Rebuttal: The Heart of Your Appeal
This is where you go head-to-head with the insurer's reasoning. Pull out that denial letter and use it as your guide, addressing their points one by one.
If they denied the claim because the treatment was "not medically necessary," this is where you bring in your doctor’s Letter of Medical Necessity. You'll want to reference specific findings from your medical records to back it up.
Use clear, direct language. For example: "Your denial letter dated [Date] states the procedure was not medically necessary. However, as documented in the enclosed letter from Dr. [Doctor's Name], this treatment was essential to prevent further complications from my diagnosed condition."
The Conclusion and Call to Action
Wrap things up with a clear and unmistakable request. Don't leave any room for interpretation.
State it plainly: "Based on the evidence provided, including the specific terms of my policy, I request that you reverse your initial decision and approve payment for claim number [Your Claim Number]."
Finally, list every single document you've enclosed (e.g., "Enclosures: Letter of Medical Necessity from Dr. Smith, Medical Records from Jan 10 to Feb 15, Itemized Hospital Bill"). This acts as a handy checklist for the reviewer and makes you look incredibly organized.
Always send your appeal via certified mail. That little piece of paper proving they received it is worth its weight in gold. Following these steps gives you the best possible shot when you need to appeal an insurance claim denial.
Navigating the Appeals Process and Escalation Paths
Sending off that perfectly crafted appeal letter feels like a huge win. And it is. But it's often just the start of the journey. The insurance appeals process is a multi-stage affair, and getting a handle on each phase is the key to knowing what to expect and what your next move should be—especially if that first "no" is followed by another one.
The whole system is designed with checks and balances. Your first stop is an internal appeal, where you're asking the insurance company to take a second look at its own decision. If they dig in their heels, you can move on to an external review, where a totally independent third party gets the final word.
The First Hurdle: Your Internal Appeal
Your initial appeal is handled completely inside the insurance company. Once you send your letter and all your supporting evidence, your case gets handed to a new reviewer who had absolutely nothing to do with the original denial. This is a crucial requirement meant to give your claim a fresh, unbiased evaluation.
This new reviewer will go over everything you sent, comparing it against your policy details and the original reason for the denial. The process can take a few weeks, and you’ll get a written decision once they've made a final call.
Don't get discouraged if you find yourself at this step. Data from the Kaiser Family Foundation shows that initial internal appeals have a success rate of about 44%. That means for nearly half of the people who appeal, a well-argued case with solid proof is all it takes to overturn a denial. No more steps needed.
When to Escalate to an External Review
So, what happens if the insurer sticks to its guns? You'll get a letter called a "final adverse benefit determination." This letter is your official green light to request an external review. It's a powerful tool that many expats don't even realize they have.
An external review takes your case completely out of the insurance company's hands. It's handled by an Independent Review Organization (IRO), a certified third party with zero connection to your insurer. Their only job is to provide an impartial, legally binding decision based on the medical facts and the fine print of your policy.
You’ll have a strict deadline to request an external review, usually somewhere between 60 to 120 days after getting the final denial. Missing this window can mean losing your right to this critical step, so you have to act fast.
This is where persistence really starts to pay off. While that 44% success rate for internal appeals is pretty good, the data shows that of the cases that get escalated to an external review, another 27% are overturned in the policyholder's favor.
Other Escalation Paths to Consider
If the external review doesn't go your way, or if it isn't an option for your particular plan, you still have other avenues. Your situation might call for one of these strategies:
- Filing a Complaint: You can file a formal complaint with the relevant regulatory body. If your policy is U.S.-based, this would be a state's Department of Insurance. For other policies, it would be an equivalent international ombudsman service. These agencies keep an eye on insurer conduct and can investigate shady practices.
- Legal Action: Taking your insurer to court is the final resort. It's an expensive and long road, but for very high-value claims or in clear cases of misconduct by the insurer, it might be the only way forward.
The numbers around appeals are pretty shocking. In 2021, a staggering 99.8% of 48 million denied in-network claims in the U.S. were never appealed at all. Yet, for the small fraction who do fight back, over 54.3% of denied claims are eventually reversed, often after multiple rounds of appeals. These numbers prove there's a huge opportunity for expats willing to see the process through. You can dive deeper into these insurance denial statistics and appeal success rates.
Trying to manage these stages—especially across different time zones and legal systems—can feel completely overwhelming. This is where a dedicated broker from a firm like Expat Insurance becomes an invaluable partner. They can manage deadlines, handle the back-and-forth, and make sure your case is presented as effectively as possible, at every single level.
Questions We Hear All the Time About Claim Denials
When you're trying to figure out an insurance appeal from another country, it's completely normal for your head to spin with questions. The whole process can feel opaque, and the stakes are obviously high. Getting straight answers is the only way to move forward and build a case that actually works.
We've pulled together the most common questions we get from expats when that dreaded denial letter shows up. This is your quick-reference guide to the details that can make or break your appeal.
How Long Do I Have to Appeal a Denial?
This is, without a doubt, the most critical question. There's no single answer, and insurers are incredibly strict about their deadlines. Miss this window, and your chances of overturning the decision pretty much disappear.
Generally, you'll have somewhere between 60 and 180 days from the day you get the denial letter to file your first internal appeal. The exact timeframe will be spelled out in that denial notice and buried somewhere in your policy documents. The first thing you should do is find that date and circle it on your calendar—big and red.
Pro Tip: Don't wait. Getting medical records from a clinic overseas, tracking down translations, and writing a solid, persuasive letter all take more time than you think. Kick off the process the moment you get the denial to avoid a mad dash at the end.
Missing the deadline is the simplest way to lose an appeal before you even start. Insurers have very little wiggle room on this; it's a contractual thing.
What Happens If I Miss the Appeal Deadline?
Honestly, your options get pretty bleak. If you blow past the deadline for the internal appeal, the insurer's decision is usually considered final. You lose your right to challenge it through their standard process, and that includes any chance of an external review later on.
There might be some incredibly rare exceptions for truly extraordinary circumstances, but you absolutely cannot count on that. It's why acting fast is so crucial. Once that window shuts, your only path forward is probably expensive and complicated legal action—a true last resort with zero guarantees.
Can My Doctor's Office Appeal for Me?
Yes, and having them do it can be a massive advantage. Your doctor or clinic has all your medical records on hand and can explain the clinical necessity of your treatment far better than you ever could. Many clinics, especially those used to working with expats and international insurance, have people on staff who do this all the time.
But don't just assume they'll take care of it. You have to be proactive.
- Give them formal permission: You’ll almost certainly need to sign a consent form that allows them to talk to your insurer and act on your behalf.
- Stay in the loop: Hand them a copy of your denial letter and any other communication you've had. Then, follow up to make sure the appeal was actually submitted correctly and on time.
Even when your doctor's office handles the paperwork, remember: it’s your appeal. The final responsibility for hitting deadlines and ensuring the information is right still falls on you.
How Can an Insurance Broker Help Me Appeal?
An insurance broker can be the most powerful person in your corner during this fight. Your doctor focuses on the medical side of things, but a broker is an expert in insurance policies, confusing procedures, and the art of negotiation. A great broker, particularly one who specializes in expat insurance, becomes your official advocate.
When you bring in a dedicated broker, they can:
- Dissect Your Denial and Policy: They'll tear apart the insurer's reasoning and check it against the fine print of your policy to find the weak spots and build a case.
- Run the Whole Show: From chasing down documents to writing the appeal letter and managing every phone call and email with the insurer, they lift that entire administrative weight off your shoulders.
- Know When and How to Escalate: If the first appeal doesn't work, they know exactly what buttons to push to start an external review or file a formal complaint with the right regulator.
Just having a broker involved sends a clear signal to the insurance company that you're serious and you know your stuff. That alone can dramatically improve your odds.
What Are the Top Reasons Appeals Fail?
Knowing why appeals get rejected is the key to not making the same mistakes. While every situation is different, most failed appeals stumble into a few common traps.
Here are the most frequent reasons an appeal goes nowhere:
- Not Enough Proof: The appeal didn't have enough hard, objective evidence to dismantle the insurer's reason for denial. This is a big one for "not medically necessary" denials, where a detailed letter from the doctor was missing.
- Missed Deadlines: Simple as that. The appeal was sent in after the strict deadline mentioned in the denial letter.
- Arguing the Wrong Point: The appeal letter was just an emotional vent instead of a structured, point-by-point takedown of the specific reason they gave for the denial.
- Missing Paperwork: The appeal was incomplete. It was missing something essential like the original denial letter, key medical records, or even the claim number.
If you methodically avoid these pitfalls, you can build a professional and compelling case that gives you the best possible shot at turning that "no" into a "yes."
Trying to fight an insurance claim denial while living abroad is a tough battle, but you don't have to go it alone. The expert brokers at Expat Insurance are here to be your advocates, handling the entire appeals process so you can get back to your life. We compare plans from over 65 insurers to find you coverage you can actually rely on, backed by 24/7 support. Get your free quote today and discover the peace of mind that comes from having an expert on your side.
Get Protected While Living Abroad
Found this article helpful? Make sure you have the right insurance coverage too. Get instant quotes for international health, life, and travel insurance.
Takes 2 minutes • Compare multiple providers • Expert advice

